Why hidden PAD matters
Peripheral arterial disease often progresses silently until patients present with advanced ischemic symptoms. Many cases remain undiagnosed because claudication is subtle or absent, and physical exam alone lacks sensitivity. Missed detection carries serious consequences: PAD is a marker of systemic atherosclerosis and is strongly associated with elevated cardiovascular morbidity and mortality. Identifying disease before it becomes symptomatic allows clinicians to intervene earlier with medical therapy, lifestyle modification, and risk reduction.
Limitations of routine evaluation
Palpation of pedal pulses and inspection for trophic changes remain part of the bedside exam, but these findings have limited predictive value. Claudication is frequently underreported by patients who attribute exertional leg pain to neuropathy, arthritis, or aging. Traditional ankle-brachial index performed with Doppler is an established screening tool, but it is underutilized in primary care due to equipment, training, and workflow constraints. As a result, many at-risk patients are not assessed until they present with advanced vascular compromise.
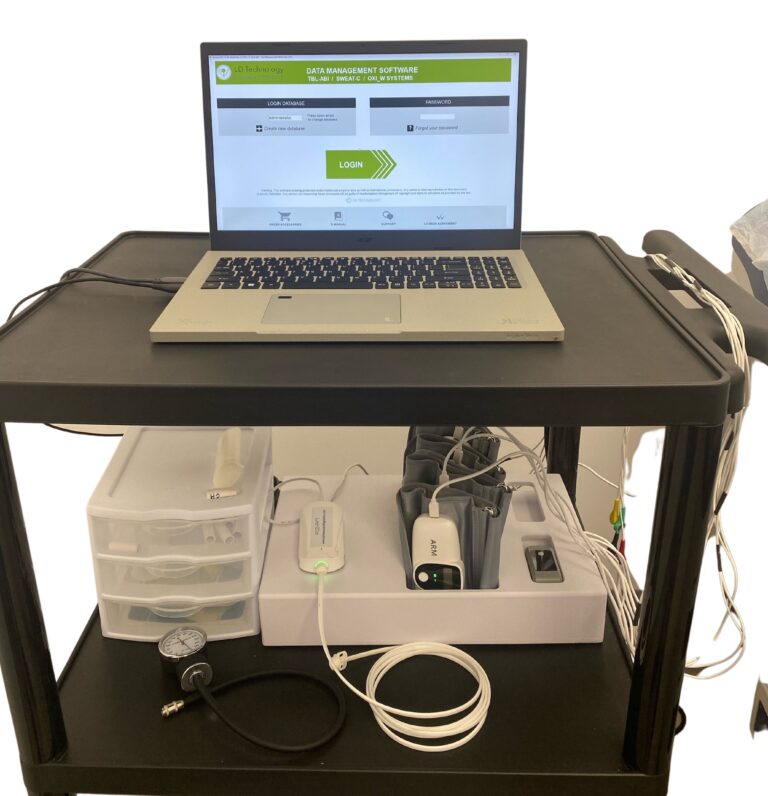
How the TM Flow System contributes
The TM Flow System incorporates ankle-brachial index into its multimodal physiologic testing. By integrating plethysmography-based ABI with sudomotor and autonomic assessments, it allows clinicians to capture large-vessel perfusion data in the same session that evaluates neuropathic contributions. This integration is particularly valuable in patients with diabetes or metabolic syndrome, where neuropathy and vascular disease frequently coexist.
Detecting early disease in high-risk groups
The TM Flow System makes it practical to assess vascular status in the office, even in patients who may not report classic claudication. A reduced ABI, particularly values at or below 0.90, supports the presence of PAD and should prompt guideline-directed evaluation and management. In patients with borderline or normal ABI but persistent symptoms, the report highlights where further vascular laboratory assessment may be indicated. Detecting PAD before it becomes clinically obvious enables earlier intervention to reduce cardiovascular risk.
Interpretation in context
As with all physiologic testing, results must be interpreted in light of the full clinical picture. ABI may be unreliable in advanced diabetes or chronic kidney disease due to arterial calcification. In such cases, toe-brachial index or referral to a vascular laboratory may be required. The TM Flow System provides physiologic signals that enhance diagnostic precision, but it is not a substitute for clinical judgment or guideline-based evaluation.
Practical implications for primary care
Integrating PAD assessment into a single session that also evaluates neuropathy and autonomic function makes testing efficient and accessible. Clinicians can use the results to direct further workup, document baseline vascular status, and tailor management. In patients with diabetes, hypertension, hyperlipidemia, or smoking history, the ability to identify subclinical PAD in the office enhances risk stratification and justifies intensification of preventive therapy.
Strengthening documentation and follow-up
The TM Flow System generates structured reports that can be included in the chart and compared over time. This facilitates longitudinal monitoring of vascular status, supporting decisions on therapy escalation, referral, and patient education. For insurers and care teams, objective documentation of ABI provides clear evidence of vascular assessment in at-risk populations.
By embedding ABI into a broader physiologic testing platform, the TM Flow System helps primary care physicians detect hidden PAD before it becomes clinically overt. The result is earlier identification of vascular risk, improved documentation, and clearer decision making for high-risk patients.